What Stands in Our Way: The Third Molar (Wisdom Teeth)
Introduction:
According to Wikipedia, the definition of wisdom is as follows
“Wisdom, sapience, or sagacity is the ability to think and act using knowledge, experience, understanding, common sense and insight”.
So that got me thinking, are we using our wisdom when it comes to the third molars? Are we all thinking along the same lines as specialist professionals, or do we have ‘specialisation bias’ based on our dental nurturing? There is no doubt that guidelines help us all think in the same way: to have some consistency and uniformity. However, it is all based on the notion that the guidelines hold weight. For the guidelines to be robust and have longevity it needs to be regularly updated. We also always need to take a look at the BIGGER picture.
The National Institute of Heath and Care Excellence (NICE), first published in March 2000, called for an end to prophylactic removal of wisdom teeth in the National Health Service (NHS). NICE argued that based on available evidence, there was no clinical indication of 44% of third molar removals. This would equate to a financial saving of approximately £5million for the NHS at the time. These initial guidelines started a ‘watch and wait’ approach and a reluctance to be proactive in the removal of wisdom teeth. This led to problems occurring later and in essence doctors/surgeons had to deal with more complex extractions.
Most practicing dentists have trained in the NHS at one time or another and whether we like it or not there must have been a subconscious bias in our thought process’ or at least there was in mine until I started to have more insight. What you see is what you know.
A Cochrane review in 2016 concluded a lack of evidence for the NICE guidelines at the time of publication. They noted that the emphasis of the NICE guidelines was based on the risks of surgery but ignored future pathology.
From my own professional bias, I believe the NICE guidelines also ignore a huge topic: treatment of occlusal problems (#orthodontics).
In the following article I will go through some real cases with my take on the third molars. I appreciate that there are many factors to consider in each case but I cannot put a full history and records in this article so we will be mainly looking at the panoramic radiographs. I certainly do not expect that everyone will agree 100% with my thought process, however, I hope there is some logic to the conclusions for each case.
What is my reasoning for removal of the wisdom teeth?
Pain, infection, caries, fracture, pathology.
Mesioangular impaction on the second molars. Remove them to prevent distal surface caries (DSC): especially impactions on lower second molars.
Over erupted upper third molars which are non-functional and will not have an opposing tooth/prosthesis.
Unhygienic and non-functional.
Lack of space in the arch: Third molars will remain in a partially erupted position; if orthodontic up righting of the posterior segment is required (therefore distal movement of molars will be required).
Pure distalisation of second molars for occlusal correction, vertical control, particularly in anterior open bite cases (the use of skeletal anchorage has opened the option of distalisation of individual teeth, segments, or the entire arch).
Class 3 cases where the overbite is reduced and the lower third molars will most likely cause further reduction in overbite due to mesial drift (clinical observation shows this to be true).
Orthognathic surgical cases where levelling of the curve of Spee is required and the wisdom tooth is in line with the surgical cuts.
When upper third molars are causing, the upper second molars to rotate/tip such that there is an occlusal interference with the palatal cusps of upper second molars. This leads to an unstable bite/CO-CR discrepancy. This along with tooth wear is a sign not to ignore.
Case 1 Example
48 YEAR OLd FEMALE SEEKING INVISALIGN TREATMENT.
Thoughts:
There is one remaining third molar: lower left.
The lower left third molar has over erupted
Invisalign will not intrude this tooth mechanically.
The lower left first and second molars have been root filled. If the patient were to lose one of these teeth, she has stated that she will not have fixed orthodontics so will likely have a bridge / implant.
The extraction would be straight forward / conical root.
The upper left second molar will not be nonfunctional.
Lower second molars will need up righting as part of the orthodontic plan.
Conclusion:
Asymptomatic although the lower left third molar should be removed to achieve treatment goals and long-term stability.
Case 2 Example
45 Year old female started to get pain in the lower right quadrant
Thoughts:
• Horizontally impacted lower right third molar causing distal surface caries on the lower right second molar; severe. Needs urgent attention.
• The upper right third molar will be non-functional.
• There is lack of space and the third molars on the left should be strongly considered for removal.
• The upper left second molar has a large restoration so if the patient may have future orthodontics the upper left wisdom tooth could be maintained. This should be discussed with the patient.
Conclusion:
• Early removal of third molars would have avoided this situation. Especially the lower right.
“The impediment to action advances action. What stands in the way becomes the way. ”
Case 3 Example
24 year old wanting to correct relapse with invisalign
Thoughts:
The left third molar has been removed, the upper and lower right third molars remain.
The overbite is reduced.
The occlusion is class 2 on the right (side of third molars).
There is lower incisor labial recession (the lower incisor is forward out of bone).
The lower right third molar is partially erupted, hard to clean.
The lower right third molar is mesiangular and impacting on the second molar.
The upper right third molar is non functional.
Conclusion:
The upper and lower right wisdom teeth are asymptomatic but should be removed for treatment goals and long-term occlusal stability and to prevent future pathology/caries.
Mechanically, it is not possible to upright the upper and lower right molars with the wisdom teeth in position.
Case 4 Example
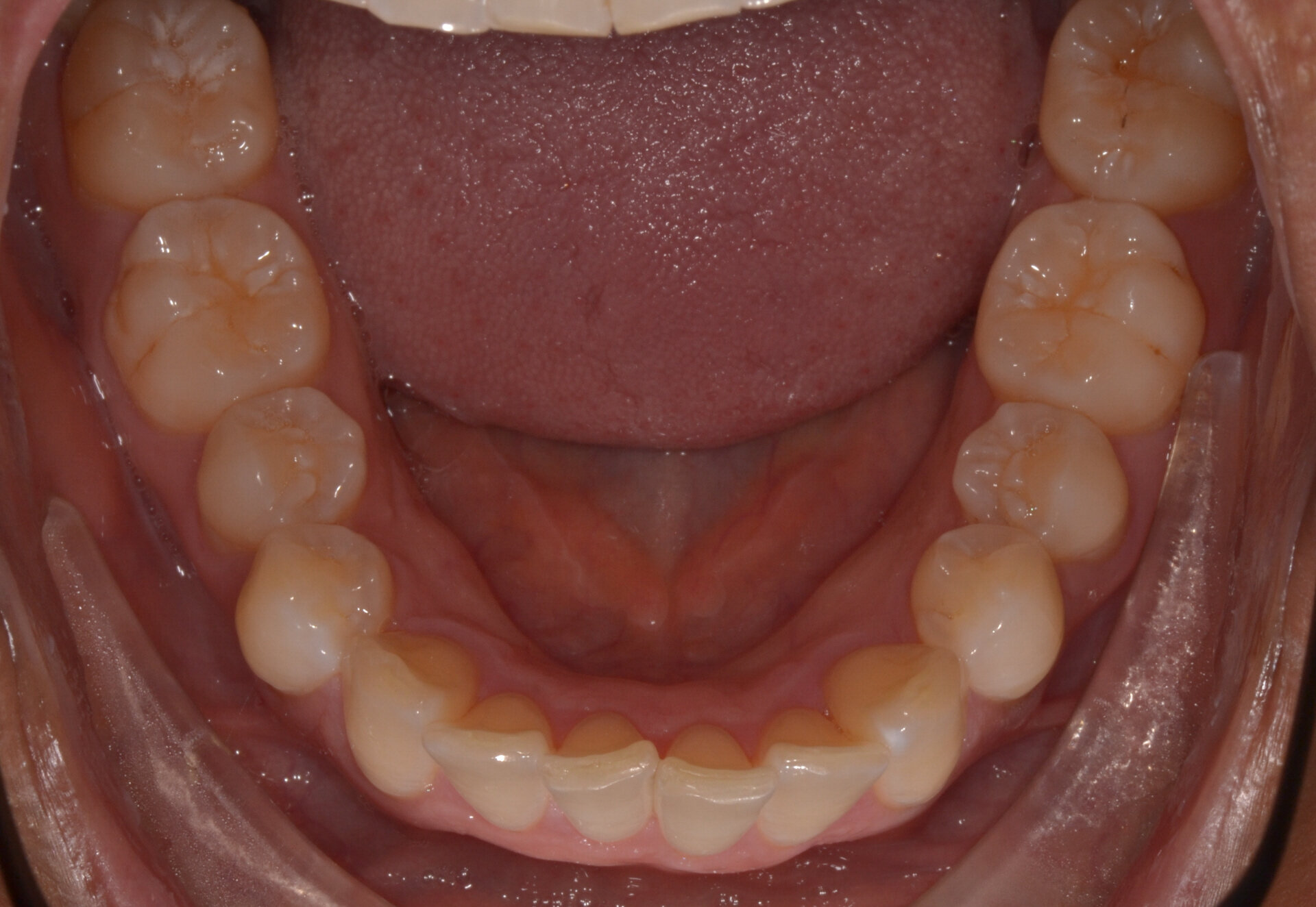
32 year old female wanted lingual braces for alignment
Thoughts:
Wide arch and all third molars erupted but crowding exists. There is a lack of space.
The upper third molars are distally inclined indicating crowding.
Lower right third molar is mesioangular and will not be uprighted orthodontically.
The posterior segments will need uprighting.
There is lower incisor crowding with flared and tipped lower incisors.
Thin biotype.
Conclusion:
I requested removal of all four asymptomatic third molars before orthodontic treatment started.
The lower third molars were removed and upper third molars were left by surgeon. Post treatment radiograph shows overrupted upper third molars.
I would still recommend their removal. Re-refer.
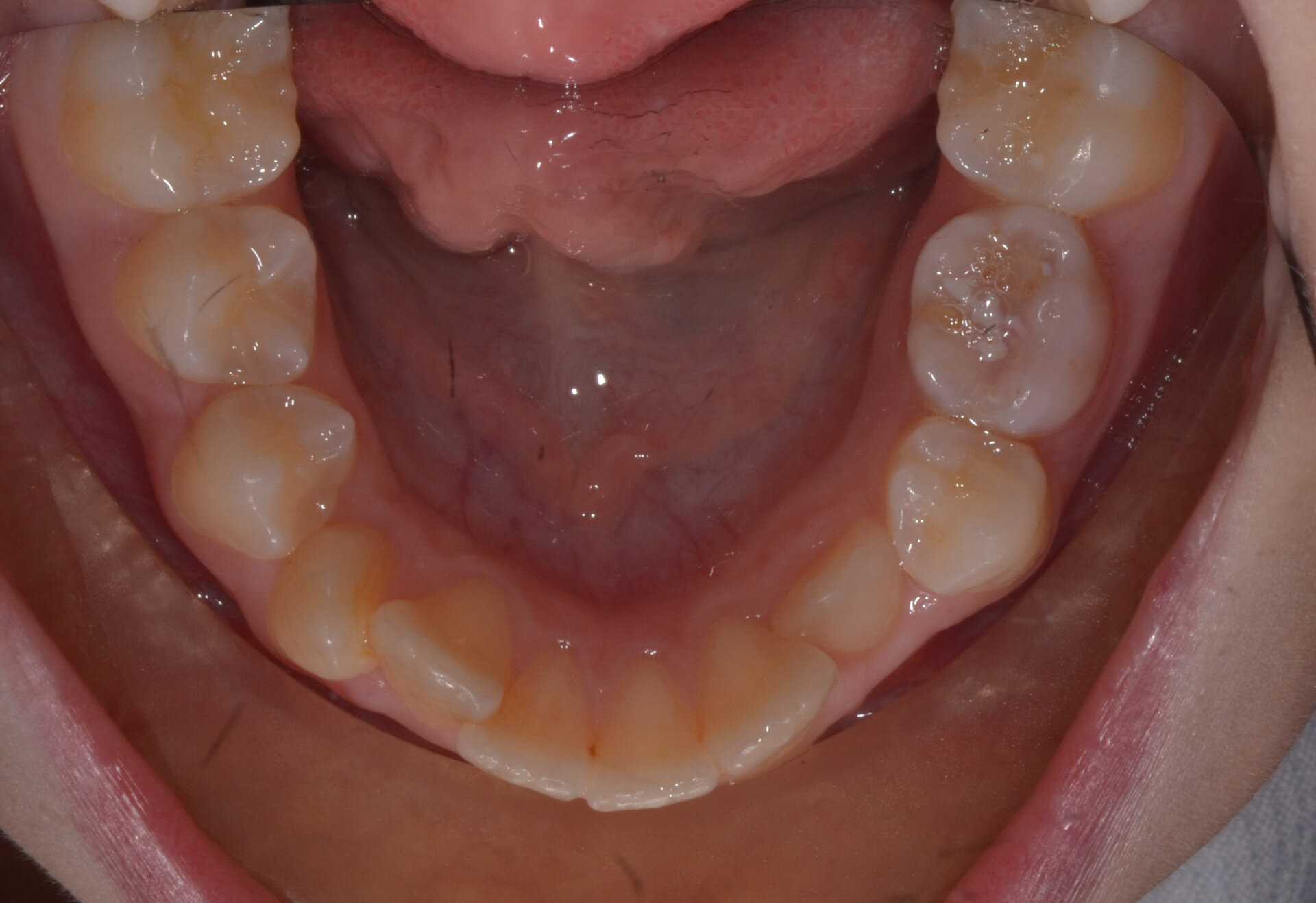
Case 5 Example
33 year old male concerned about anterior open bite
He had previous orthodontic treatment with four premolars removed as a teenager. Re-treatment required.
Thoughts:
The posterior teeth will need uprighting.
There were premature contacts on the posterior teeth/CO-CR slide.
Tooth wear evident and lower incisor crowding.
Although the third molars were erupted and functional they would require removal to correctthe bite and improve the occlusal function.
Intrusion of the third molars could be done with bone anchor miniplates but predictability is notcertain in this case, this is also a re-treatment so we want to be sure.
Conclusion:
NICE guidelines would not allow this but the third molars need to be removed to achieve occlusal treatment goals. I requested removal of all asymptomatic third molars for orthodontics.
Progress photos below:
Case 6 Example
35 Year old female seeking to straighten teeth
Thoughts:
The lower third molars are unerupted and distoangular impacted and will not erupt in good positions.
There is a general lack of space for the lower third molars.
The upper third molars are high and impacting on the upper second molars causing a significant change in their torque.
If we are to start orthodontic treatment, we will not be able to correct the second molar positions without the extraction of the upper third molars.
Long term occlusal stability would be significantly improved by removal of third molars (there is pre-exisiting molar cross bites).
Conclusion:
ALL four asymptomatic third molars should be removed before orthodontics for predictability in achieving goals and long term stability.
Case 7 Example
16 year old female post orthodontics retainer check
Thoughts:
Impacted lower third molars with mesioangular position against the second lower second molars. High risk of DSC.
Upper third molars are pushing on the roots of upper second molars. This has the potential to cause rotations and change of torque of the upper second molars leading to occlusal interferences.
Potential for periodontal/hygiene issues.
No chance the third molars will improve in position/erupt naturally.
Patient had started with lower incisor crowding and the lower incisors were proclined to compensate for the skeletal class 2 relationship. Therefore greater chance of relapse.
Conclusion:
There is a high chance of relapse.
Refer for removal of all third molars now where roots not fully formed. This could
Final Summary:
From just a few examples you can see the wide range of situations where third molars would be considered for removal.
The guidelines for removal of third molars should be broader and should incorporate the occlusal challenges that we face. We need to look at the BIGGER picture.
In my opinion early removal of third molars has greater advantages than disadvantages and should be strongly considered in many cases.
The use of 3D imaging has created a far safer diagnostic environment for the surgeon and this tool should now be commonplace for such procedures.